Courtney Pharr - Journals
Weekly Journal Entries
Home | Research | Mentor | Journal | Final Report
Week One: May 27 - June 1
After having the opportunity to explore all around Baltimore and Washington D.C. over Memorial Day weekend with my mom and
my aunt, I began work on Tuesday morning. I met with Dr. Mentis to learn a little more about her current research projects. We decided
I should focus mostly on her study with Parkinson's patients who have undergone Deep Brain Stimulation, but that I could also have the
opportunity to work on and learn more about a few of her other studies. (For more information on DBS see the above link to my 'Research' page).
In order for me to be able to work directly with patients, I needed to complete my Institutional Review Board (IRB) training. I got
settled into Dr. Mentis' lab to complete all of the necessary courses. This was a time consuming process, but it is a necessary
part of research. After I finished all of my testing for IRB approval, I got down to work analyzing videos that Rita Shewbridge
(one of Dr. Mentis' graduate students) had taken of DBS
patients during appointments to have the settings on their DBS system evaluated and, if necessary, changed. Patients generally come in every
four to six months to get their current settings checked out. Manipulating these settings can immensely
help Parkinson's patients walk, talk, and move better. The process of watching these videos was very informational for me because I was
able to see firsthand the effects that Parkinson's disease has on people's lives. The majority of my first week was spent analyzing these
videos and taking detailed notes for my mentor to use about the changes that the RN and the neurologist made in the settings and the effects
of these changes in regards to the patient's symptoms. Another major part of my first week here at UMBC was spent researching new sensors that
could potentially be used to create new technology to analyze movement in Parkinson's patients. Since Dr. Mentis does a great deal of work
with other commercial sensors, such as the Microsoft Kinect and the Leap Motion Device, she is always on the lookout for new technology.
So, after all that I survived my first week of the DREU internship, and I am looking forward to the rest of the summer!
Week Two: June 2 - June 8
Another week done of my summer internship at UMBC! On Monday and Tuesday I finished up my work from the previous
week (watching the videos of DBS patients and researching new sensors). Then on Wednesday I went with Dr. Mentis and Rita to meet with
Dr. Vandana Janeja and Dr. Ravi Kuber (also members of the Information Systems department at UMBC) to discuss areas of overlapping research.
Dr. Janeja and Dr. Kuber are studying socialization, which is relevant to Dr. Mentis' research because of the necessity of
Parkinson's patients to have social interactions and outside interests. This is so important because of the progressive nature of the disease
and the simple act of interacting with friends and family members can help Parkinson's patients live a more normal life. After this meeting,
Dr. Mentis described in more detail to me the two studies she has proposed going forward. The first is to deploy technology in the
clinic to be used to aid physicians in measuring the symptoms of Parkinson's patients, and subsequently, deploying
similar technology in the home to allow patients to test their movement ability more frequently. This would help clinicians provide better
and more accurate adjustments to patients' DBS systems. In order to more fully understand Parkinson's disease, I began reading a book that
Dr. Mentis gave me entitled, "Parkinson's Disease: A Complete Guide for Patients and Families." Reading this book has given me a better
understanding of the implications of the disease and the huge variability between the symptoms of people who have Parkinson's.
Near the end of the week, Dr. Mentis and I began looking at the different sensors that I had been researching. There are many different
sensors on the market, but not all are completely applicable to the work that we are doing. We need to keep looking further to see
what would be most useful in analyzing gait in and out of the clinic, and especially measuring freezing when patients are attempting to
step. I am excited to see what will happen for the rest of the summer and how
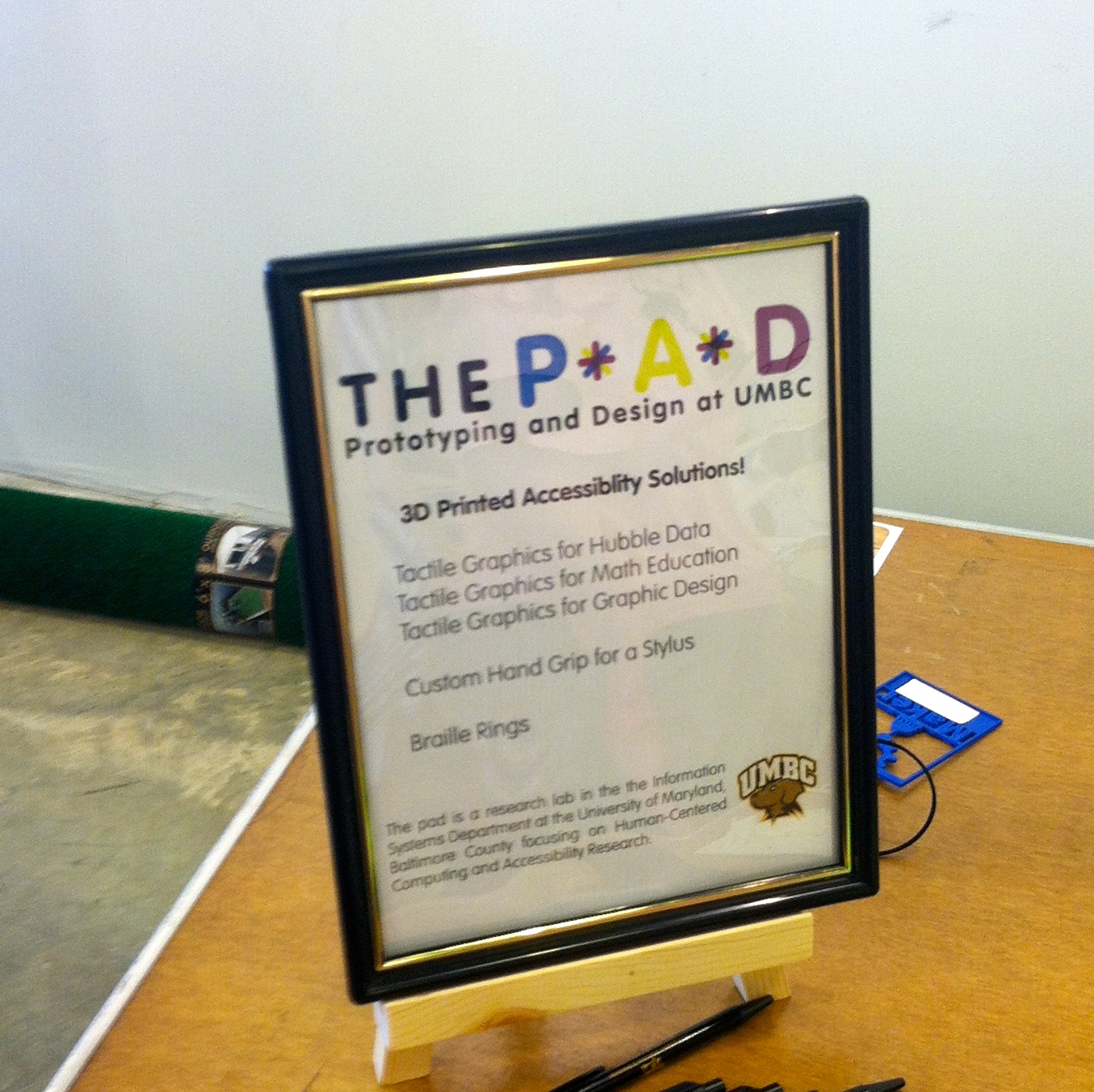
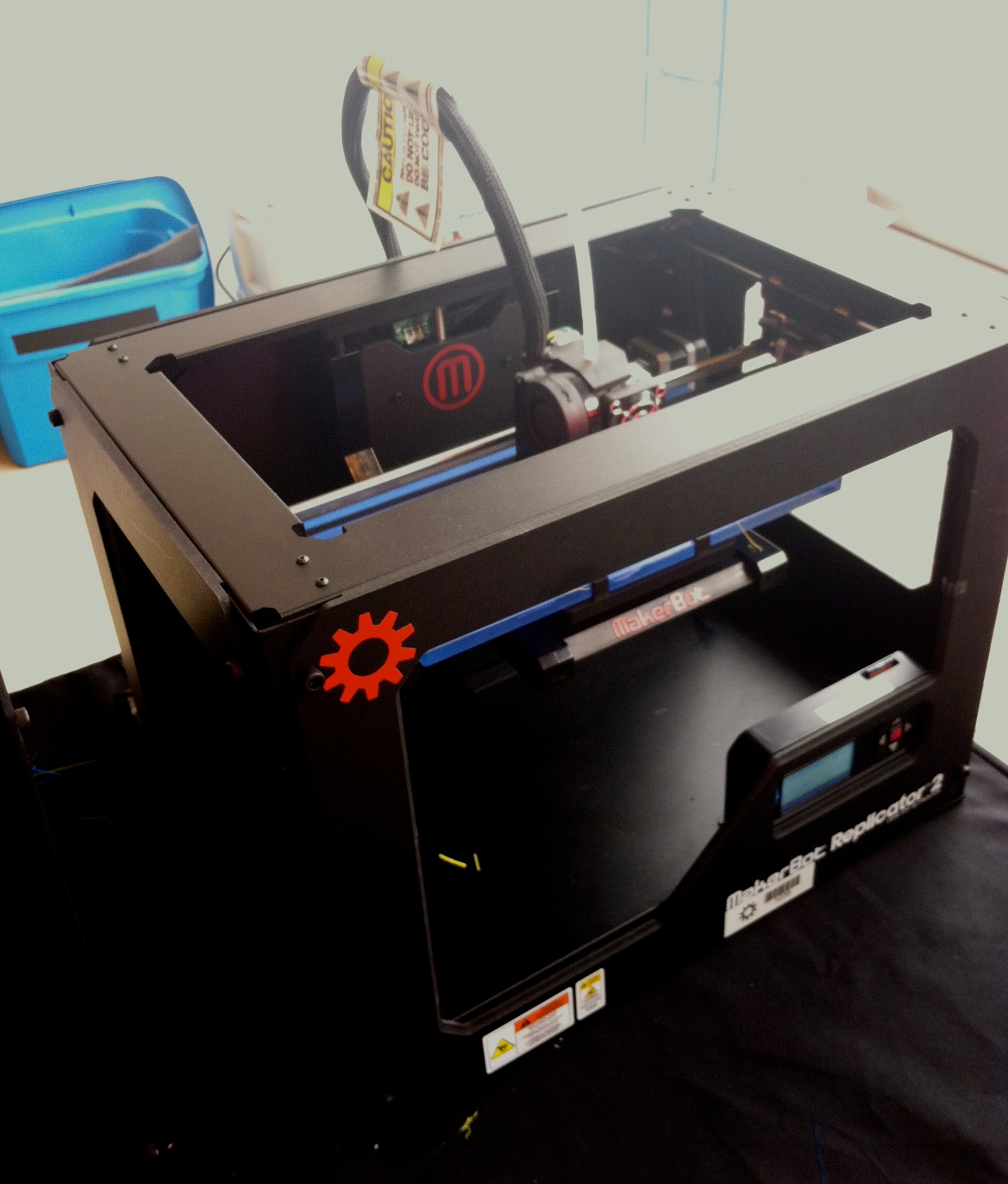
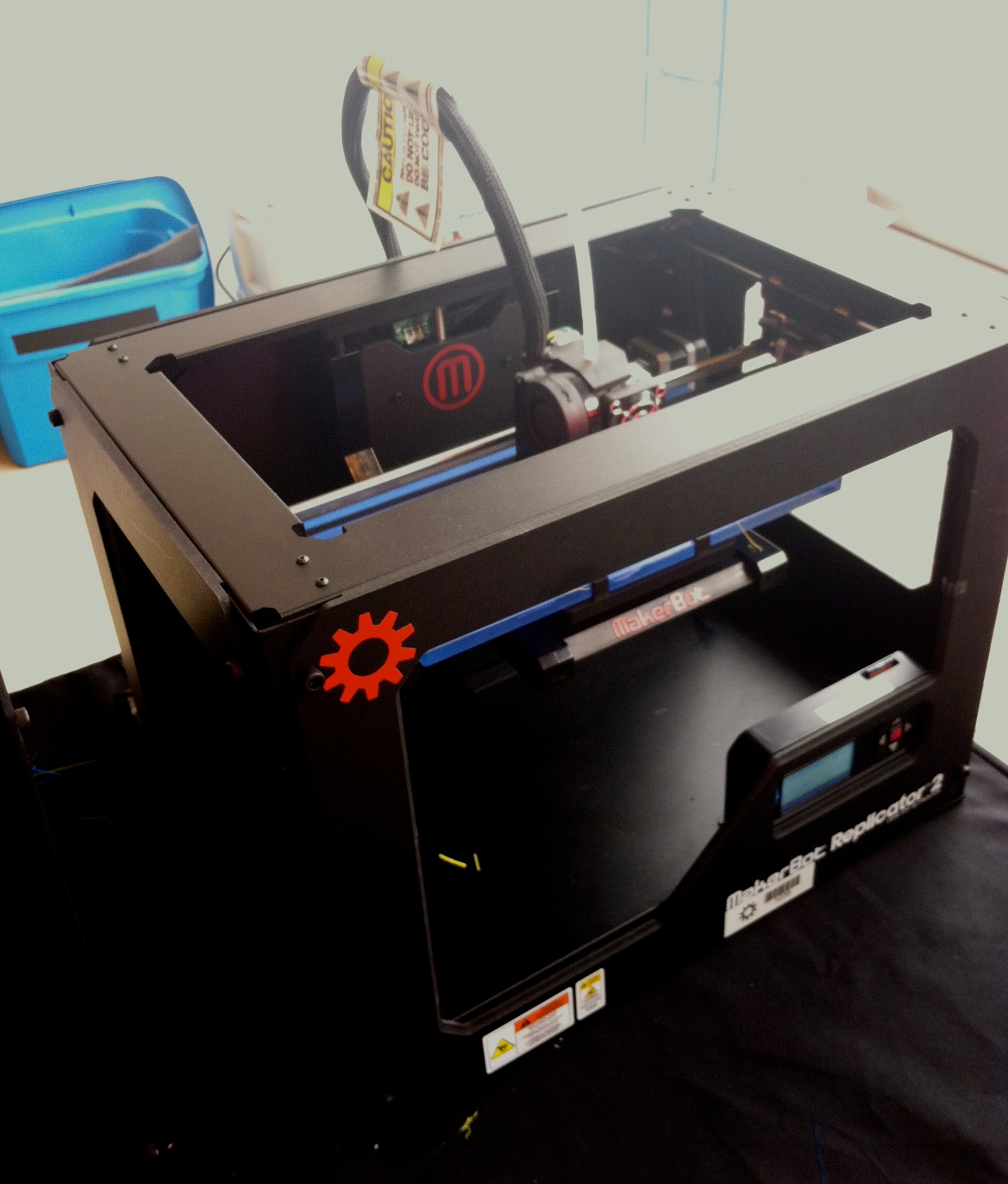
far we will be able to go with these two studies. Unrelated to my own research, over the weekend I was able to attend the DC Mini Makers Faire
with one of my roommates (Megan) who is also a DREU student at UMBC, but working with a different mentor (Dr. Amy Hurst). The purpose of
Maker faires are to celebrate learning, creativity, and new technology, such as 3D printing. The Maker movement is described as a
"tech-influenced DIY community." Dr. Hurst was presenting some of the work being done in the Prototyping and Design (PAD)
lab at UMBC in regards to accessibility research, so Megan and I went with her to help her with the booth.
I really enjoyed seeing the work of so many different people and research labs. It was a great way to wrap up the week! I've included some of
the pictures from the Maker Faire below.
 Week Three: June 9 - June 15
Week Three: June 9 - June 15
This week I worked on a literature review for
a paper that I am writing with Dr. Mentis and Rita for the
Workshop on Interactive Systems in Healthcare (WISH) 2014. I enjoyed learning how to do a literature review and learning more about
the process of writing an academic paper. The WISH conference this year is on “Interactive Systems
for Patient-Centered Care to Enhance Patient Engagement” and we are focusing on the DBS Parkinson's research. The idea of
"patient-centered care" has been around for a significant amount of time, but surprisingly little research has been done in regards to DBS.
This paper will be more of a qualitative look at this subject based on the data we have gotten from the videos. One exciting part of
the WISH conference is that they have a mentoring program for student researchers. I will hopefully be able to apply and have the
opportunity to attend the conference in November. On Thursday, Dr. Mentis and I met with Rita to discuss what we need to do for
the studies moving forward. In regards to the work we are hoping to do with the sensors and gait analysis, we will likely end up building
our own sensor using an accelerometer and an Arduino microcontroller with a Bluetooth connection instead of buying a commercial
sensor because of cost and accessibility to the raw data. However, for the time being, we are focusing our efforts on deploying
technology in the clinic to help measure the symptoms of Parkinson's
patients more effectively. Clinicians have a number of tests to check for rigidity, tremors, and other symptoms common to Parkinson's
disease. We are going to start off concentrating on the tests involving the upper body. Some of these tests include
opening and closing the hand, touching the thumb and index finger together, and holding both hands straight out to check for tremor.
What we are hoping to do is to recreate these tests using technology
in a way that allows for more objective analysis, but also allows for the patients to have a better understanding of what the clinicians
are testing. It is incredibly important for patients to be actively involved in their own care and to know why
they are being asked to do these specific tests and what clinicians are looking for with these specific movements. Hopefully
we will be able to present the data we collect in a manner that is useful for both clinicians and patients. Dr. Mentis
has a few programs that will be the basis of the technology that we deploy in the clinic. The first program is used to check for tremors.
Using the Leap Motion device, the program has a patient hold one of their hands straight out and try to keep it in a small circle displayed
on the screen. The program then outputs the x and y coordinates of the person's hand every thousandth of a second. This data
can then be used to measure a person's tremor. We are in the process of determining a baseline for what a normal amount of tremor
would be. Next week I will be able to play around with the code, clean it up, and hopefully get it closer to actually being
used to help patients! We are also hoping to create programs that will test hand opening and closing and touching the thumb
and index finger together. We will have to write these programs from scratch using the newer version of the Leap Motion device. I'm
excited to continue moving forward with these projects and to see how much I can accomplish in my time at UMBC!
Week Four: June 16 - June 22
I can't believe I have already been here for one month! On Monday of this week I finally received my IRB approval,
so I was able to go the Neurology Department of the University of Maryland Medical School to observe Parkinson's patients as they
had the settings on their DBS systems changed. It was a great experience to be able to see the immediate improvements of small DBS changes
on patients' symptoms. It was also very beneficial to be able to ask questions of the neurologist and the
RN and to be able to get their perspective on exactly what they are looking for when they make changes. One thing that really resonated
with me at the clinic was when the RN said to me that the reason she enjoyed her job so much was that when she worked with DBS patients
she was always able to make them better, even in a small way, before they left the clinic. I hope that with whatever
career I end up having I will be able to do exactly that.
For the rest of the week, I continued to work on the literature review for the WISH paper and I also went back through all of the videos
in order to get more data for the paper. I was mainly focused on transcribing any stories that patients shared with the clinicians that were
related to patient-centered care. This included sharing any symptoms or life events affecting their health
and well-being. Patient-centered care in DBS is especially important because so many of the programming changes that clinicians make are
done based on what patients say they are experiencing. It is critical that clinicians take patients' narratives and symptoms into account.
We have noticed several times in the videos where
a patient has complained of a particular symptom and the clinician will make a DBS programming change, but while the clinician will think
that the patient is walking or talking better, the patient doesn't actually feel better. This is problematic because it is not respecting
the patient's point of view, when the patient is the only person who can
feel the effects of the change in DBS programming. This is the main reason we are working to develop new
technology to deploy in the clinic to hopefully validate the patients' experiences and also present the results in a more transparent way.
Next week I will begin the development of a program to recognize when a patient's hand is open or closed (as well as the varying states
in between) since that is the test most frequently used in the clinic with DBS Parkinson's patients.
Week Five: June 23 - June 29
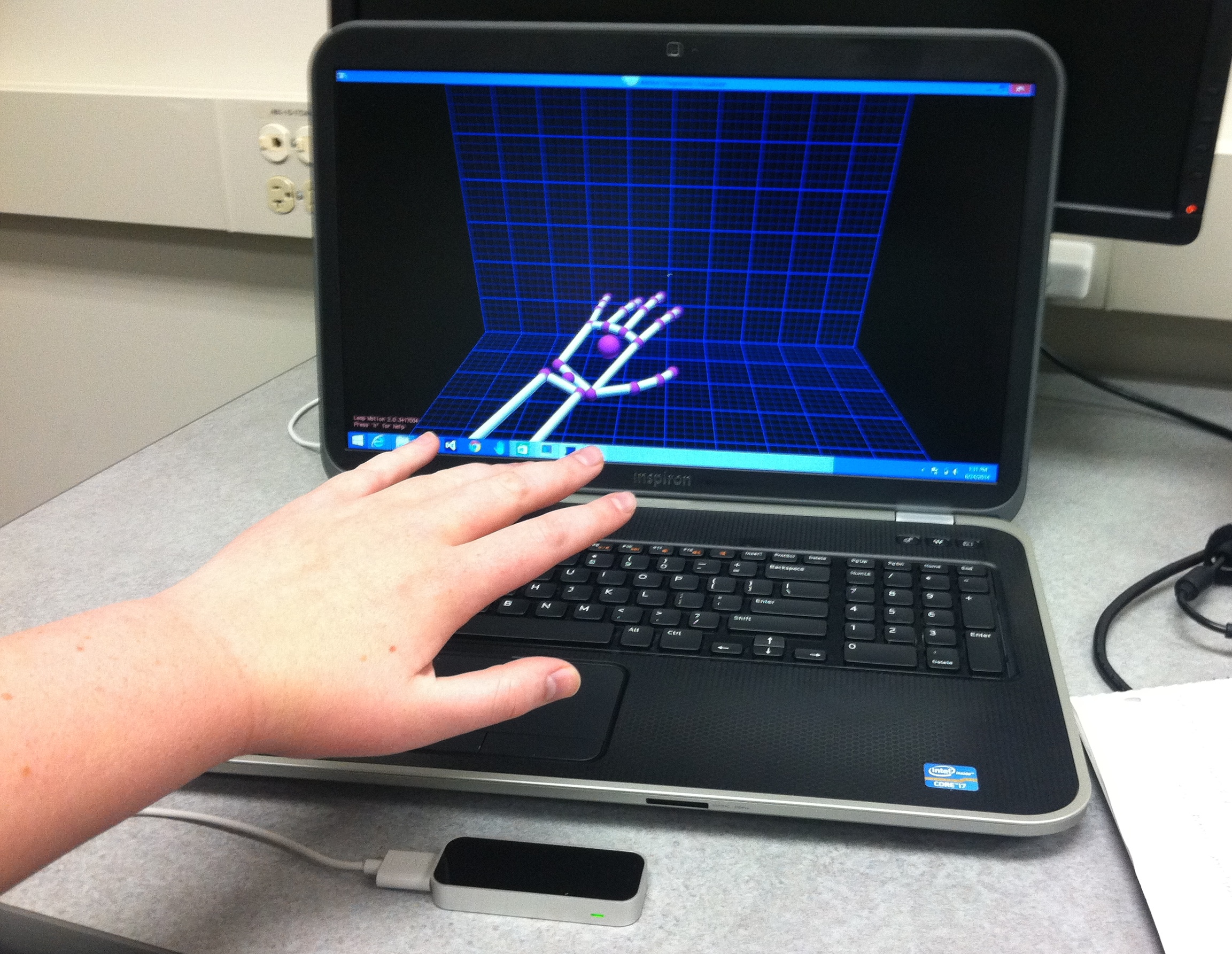
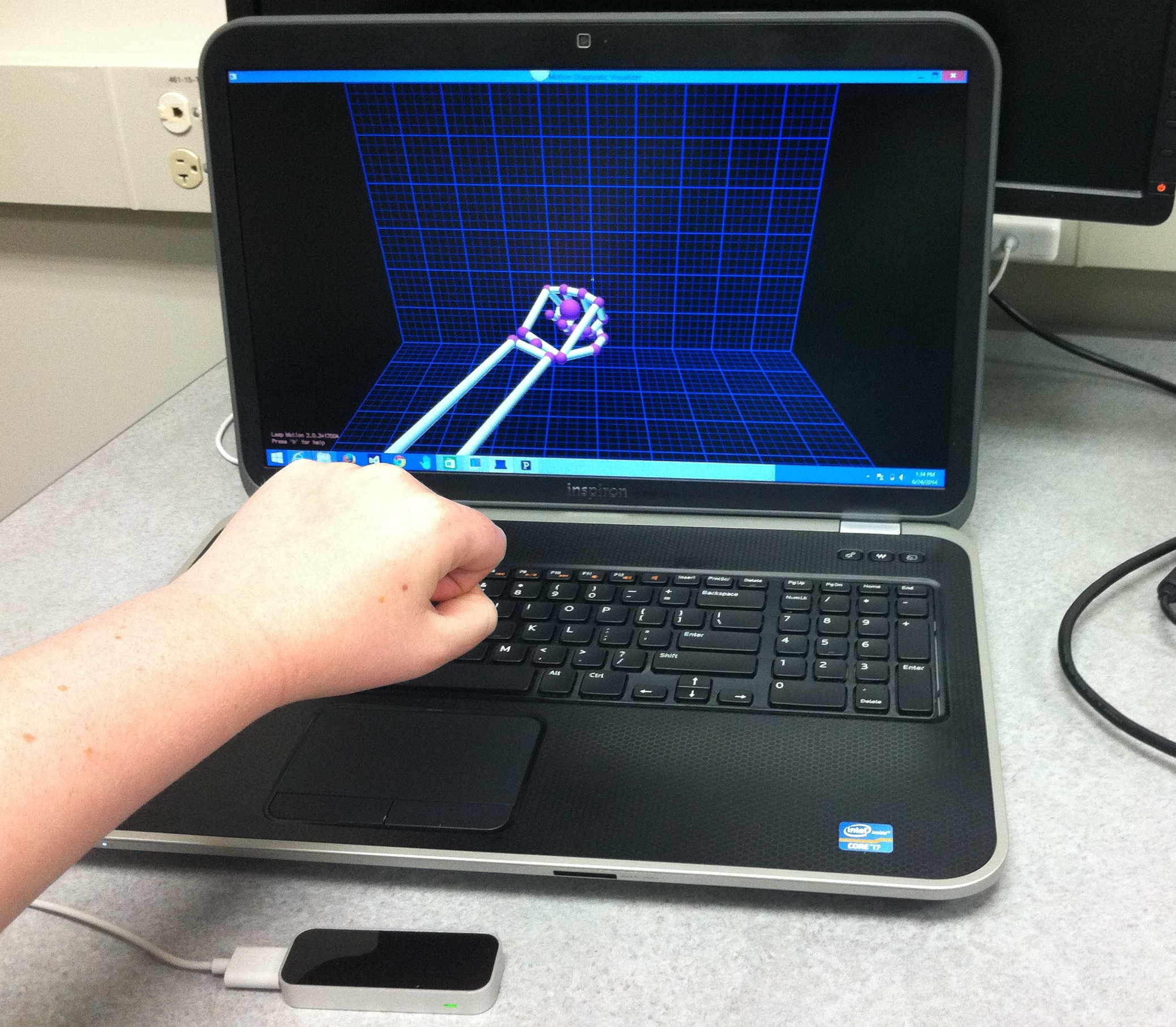
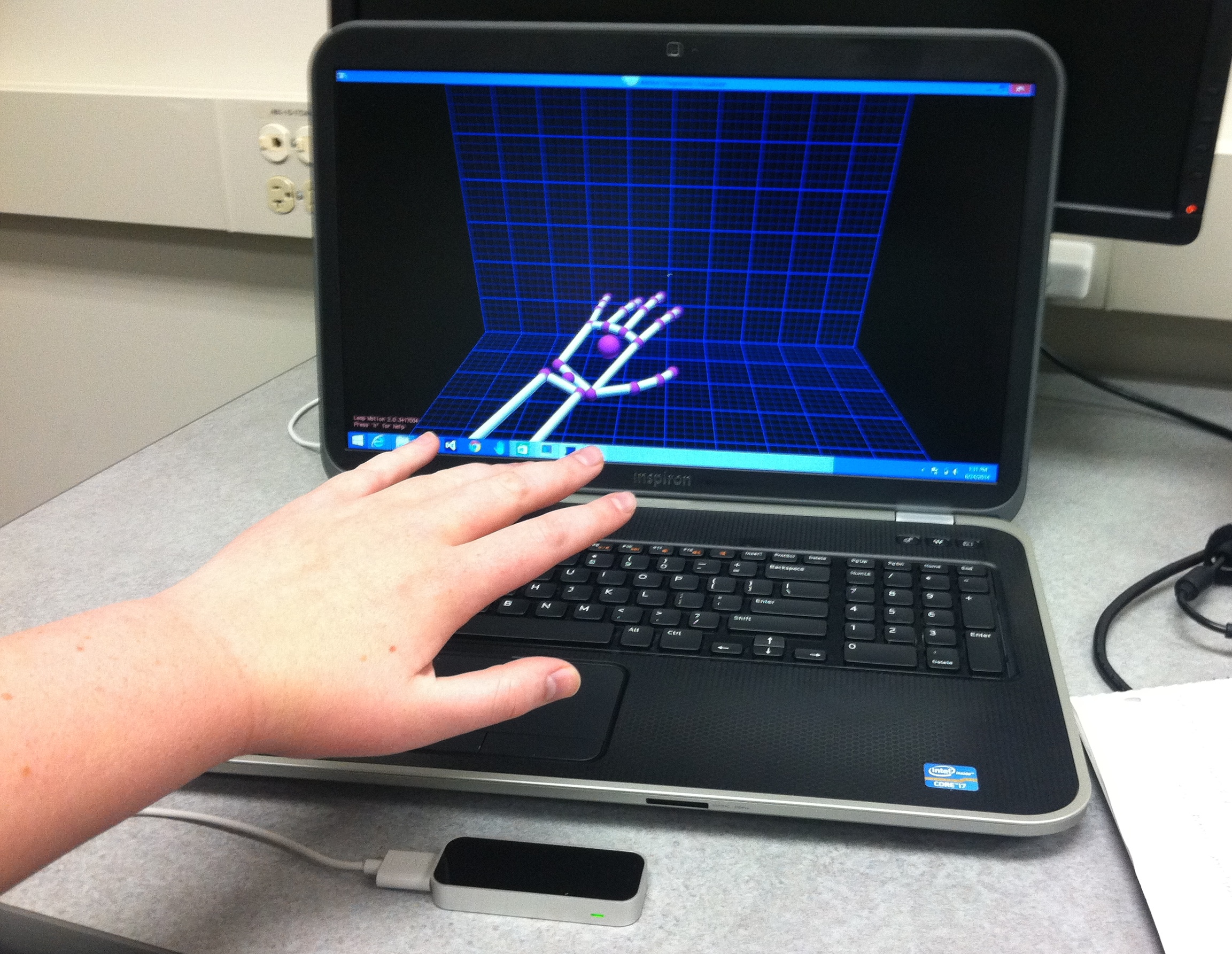
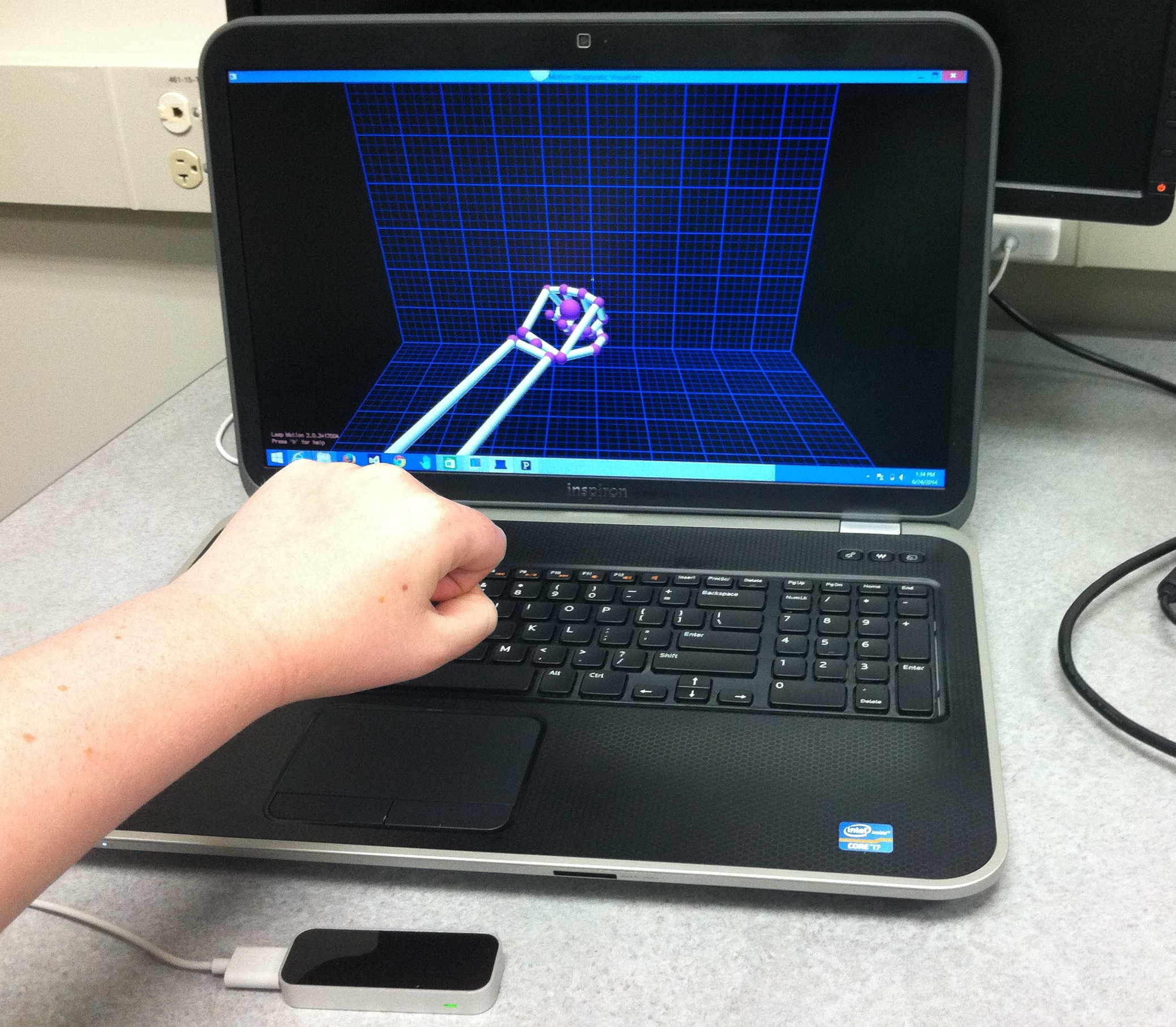
This week was exciting as I began to develop the technology that we hope to deploy in the clinic pending IRB approval.
The first test we want to replicate using technology is opening and closing the hand. To do this we are using
the Leap Motion sensor and Processing, which is a programming language very similar to Java. The newer version of the Leap Motion SDK
has a function called grabStrength(), which returns a value between 0 and 1 depending on how closed the hand is. A value of 0 represents
fully open and a value of 1 represents fully closed. I really enjoyed learning a new programming language and figuring out how it works
in conjunction with the Leap Motion device. Playing around with this technology has been so much fun and has been a nice change of pace
from the other research tasks I have been working on. I've included some pictures from Leap Motion Visualizer below!
 Week Six: June 30 - July 6
Week Six: June 30 - July 6
Time is flying by! This week I continued editing and modifying the program I had begun working on last week.
We had to make a few changes in what programming language we were
using because the latest version of the Leap Motion SDK does not have support for Processing. We decided to try
Java because it is the most similar and this is the language that I have the most experience with. The other programming languages
that the Leap SDK supports are JavaScript, Unity/C#, C++,
Python, and Objective-C. Writing this program and working to develop new technology is incredibly fun, as well as challenging.
I don't have very much experience programming with the Leap Motion device,
but it is always enjoyable for me to work through a problem until I am able to figure it out. By the end of the
week I was able to get the basic functionality of the program working. Next week I will continue making modifications and I
will begin developing the GUI to make it more user friendly.
Week Seven: July 7 - July 13
The program is up and running! I finished developing the GUI this week and made a few changes to the output of the program.
The user can now start and stop collecting data from the java applet when the test subject begins opening and closing
his/her hand. The applet also includes an area to enter the Patient ID number, has an option to select whether this test is pre or post
any DBS programming changes, and includes a button to manually count the number of times the test subject closes his/her hand.
This will hopefully allow us to validate our own system. Since the Leap Motion grabStrength() method is relatively new with the latest
version of the Leap Motion SDK and still untested, we want to verify the data we are collecting because the sensor is not perfect. The
program outputs the grabStrength() data and the time in milliseconds to a CSV file. We will then be able to determine whether the test
subject can open and close his/her hand all the way, the speed of opening and closing, and the
variability or fatigue (does it take the test subject significantly longer to open and close his/her hand the longer they do the test).
We hope to present this information graphically in a way that is beneficial to clinicians, but especially helps the patients.
I also continued to help Rita with the WISH paper this week. I am quickly learning that the hardest part of writing an academic
paper is narrowing down your topic and synthesizing the vast amounts of data that you have.
Week Eight: July 14 - July 20
This week, in addition to finishing up the WISH paper, I began working on the literature review for another paper that Rita and I
are writing for the conference on Tangible, Embedded, and Embodied Interaction (TEI). We
are planning to design and build a prototype for a personal wellness device using the laser cutter in the PAD lab. I am excited
because this is very different from everything else that I have been working on this summer. I also spent part of this week testing out
the program. The Leap Motion device is not perfect, but overall we found the data that it collects fairly accurate and usable.
Dr. Mentis found out that we received IRB approval to add this technology to the existing IRB that we have to observe Parkinson's patients.
I am hopeful that I might have to chance to test out the technology that I have built in the clinic before my internship is over!
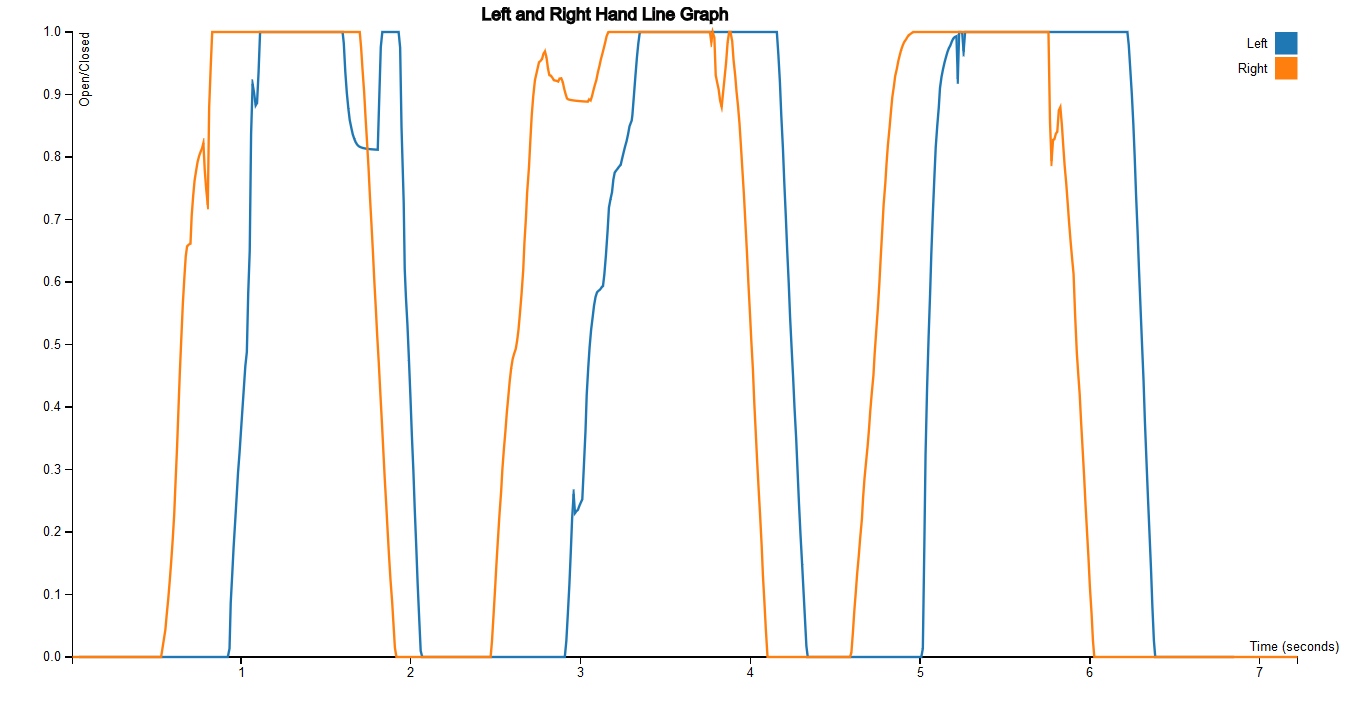
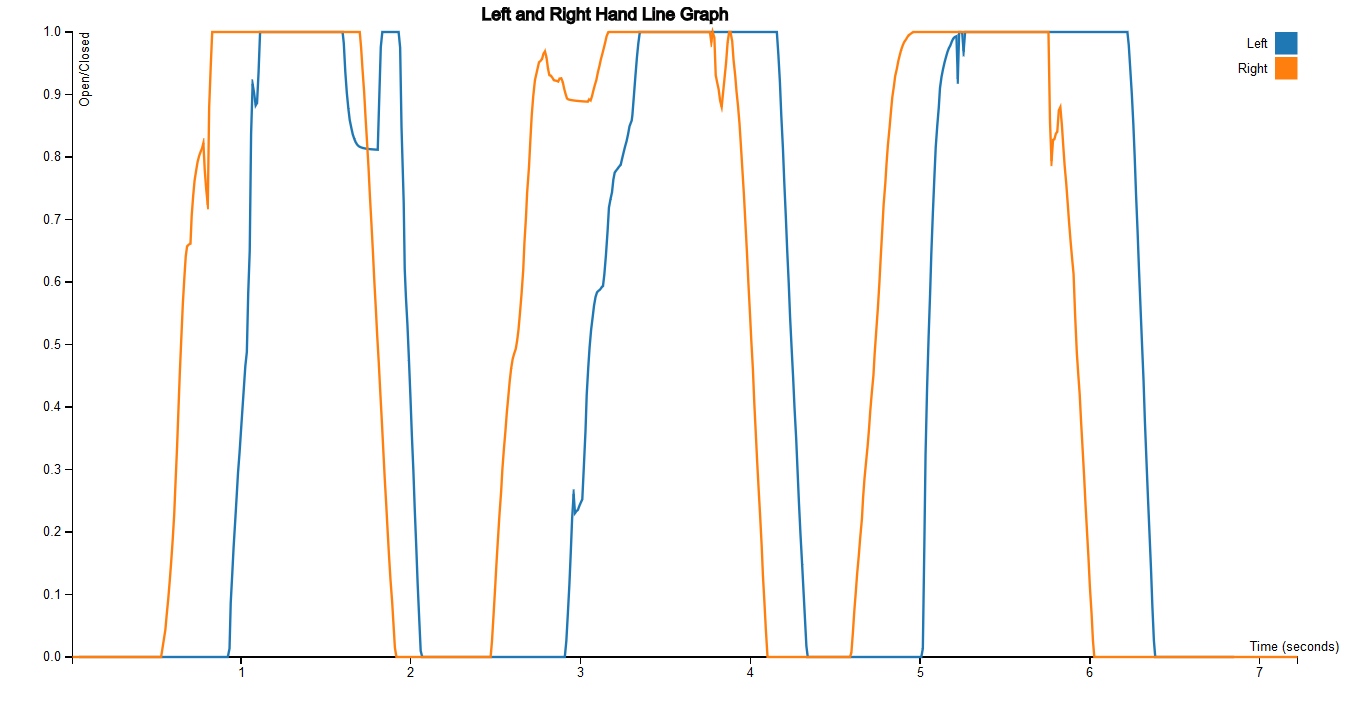
Week Nine: July 21 - July 27
WISH paper is submitted! Hopefully I will soon have my first
publication! This week I worked on an IRB protocol for an internal study that we hope to run at
UMBC. The technology that we have developed for the clinic is finished, but we are struggling
with how to present our data in a manner that can be easily understood by patients. The majority
of people have difficulty reading graphs and understanding numerical information, so we are trying
to stay way from presenting our information graphically as much as possible. Our hopes for the
UMBC study are to find out if people perceive the data that we present to them about opening and
closing their hands as accurate, and ask them how they would present this data in the simplest
manner possible. As a starting point for this study, we have created a program that will draw a
line graph based on the data collected by the Leap Motion sensor when the program is run. Although
we will most definitely need to develop other visualizations of the hand data, the line graph is a
way for us to begin the process of figuring out the most effective visualization for the in-clinic
study. Crossing my fingers that we will hear back from the IRB before the end of next week!
Week Ten: July 28 - August 1
I can't believe I have already finished my ten weeks here at UMBC! What a wonderful experience! I have learned so much and the
DREU program has made me even more excited to continue my studies in computer science. This week I worked on developing improved
visualizations for the internal study at UMBC. I created a line graph and a scatterplot graph, which compare the test subject's
left and right hands from open to closed, as well a visualization which only shows the times when the hand is closed.
This will help us to visualize the variability
between hand opening and closing to determine if the hand is becoming fatigued quickly. Hopefully these visualizations will give
us a good starting place for the study at UMBC and will allow us to get feedback from participants so we can improve our
visualizations before integrating the technology into the clinic. Although I will not have the opportunity to test out the program
I have developed before I leave, I hope to remain connected and involved with the project moving forward. I am so grateful to have
had this opportunity to become involved in research and I am excited to see where the future will take me!
 Back to Top
Back to Top